Hip Conditions
The hip joint is a ball-and-socket joint that connects the leg to the pelvis. It is one of the body's largest and most important joints, allowing a wide range of motion while supporting body weight.
Anatomy of the Hip Joint
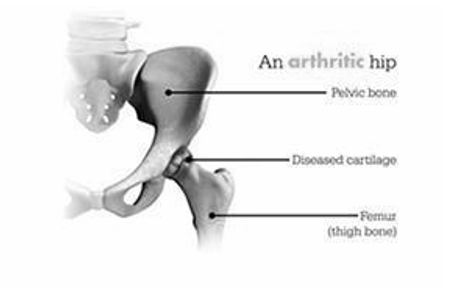
1. Bones
- Femur (Thigh Bone): The head of the femur forms the "ball" part of the joint.
- Pelvis (Hip Bone): The acetabulum is the "socket" in the pelvis where the femoral head fits.
2. Cartilage
- Articular Cartilage: Covers the surfaces of the femoral head and acetabulum, providing smooth movement and cushioning.
- Labrum: A ring of cartilage around the acetabulum that deepens the socket and stabilizes the joint.
3. Ligaments (Connect bones to bones)
- Iliofemoral Ligament: The strongest ligament in the body, preventing hyperextension.
- Pubofemoral Ligament: Limits excessive abduction (leg moving outward).
- Ischiofemoral Ligament: Helps stabilize the joint.
4. Muscles & Tendons
- Gluteal Muscles (Gluteus Maximus, Medius, Minimus): Control movement and stabilize the hip.
- Hip Flexors (Iliopsoas, Rectus Femoris): Help lift the leg.
- Adductors: Bring the leg toward the body.
5. Synovial Fluid & Bursa
- Synovial Fluid: Lubricates the joint to reduce friction.
- Bursa: Fluid-filled sacs that cushion and prevent irritation.
Functions of the Hip Joint
- Supports body weight during standing, walking, and running.
- Allows movements like flexion, extension, rotation, abduction (moving the leg outward), and adduction (bringing the leg inward).
- Provides stability while maintaining flexibility.
Causes and Risk Factors for Hip Conditions
Certain factors can increase the risk of developing hip conditions. These include:
- Age: Many hip conditions, such as osteoarthritis and hip fractures, are more common in older individuals.
- Gender: Some hip conditions, like hip fractures, are more prevalent in women, while others, such as ankylosing spondylitis, are more common in men.
- Family History: A family history of hip conditions can increase the risk of developing similar issues.
- Injury: Traumatic injuries to the hip, such as a fall or sports-related injury, can lead to hip conditions.
- Medical Conditions: Certain medical conditions, such as rheumatoid arthritis and lupus, can increase the risk of hip joint problems.
- Obesity: Excess weight places additional stress on the hip joints and can contribute to developing hip conditions.
Symptoms of Hip Conditions
The symptoms of hip conditions can vary widely depending on the specific condition, but some common signs and symptoms include:
- Hip Pain: Persistent or intermittent pain in the hip joint is a common symptom of hip conditions. The pain may be sharp, dull, or aching in nature.
- Stiffness: Individuals with hip conditions often experience stiffness in the hip joint, making it difficult to move the leg freely.
- Limited Range of Motion: Hip conditions can reduce flexibility and difficulty performing everyday activities like walking or bending.
- Swelling: Inflammation of the hip joint or surrounding tissues can lead to swelling in the hip area.
- Clicking or Popping: Some individuals may hear or feel clicking, popping, or grinding sensations in the hip joint during movement.
- Weakness: Muscle weakness in the hip and thigh can occur due to pain and reduced use of the affected leg.
- Limping: Some people with hip conditions may develop a noticeable limp while walking to alleviate pain.
Types of Hip Conditions
Painful Hip
A "painful hip" is a general term to describe discomfort or pain in the hip region. This pain can result from various underlying causes, including hip arthritis, bursitis, labral tears, or traumatic injuries. Diagnosing the specific cause of hip pain is essential to determine the most appropriate treatment.
Hip Arthritis
Hip arthritis refers to the degeneration of the hip joint's cartilage, leading to pain, stiffness, and reduced mobility. The two most common types of hip arthritis are osteoarthritis and rheumatoid arthritis. Osteoarthritis is typically associated with aging and wear and tear, while rheumatoid arthritis is an autoimmune condition that affects the joints.
Femoroacetabular Impingement (FAI)
Femoroacetabular impingement is a condition where abnormal bone growth around the hip joint can cause pain and limited range of motion. It occurs when the bones of the hip joint do not form correctly, leading to friction and damage within the joint.
Labral Tears
The hip joint has a ring of cartilage called the labrum that helps provide stability and cushioning. Labral tears occur when this cartilage is damaged, often due to injury or overuse. Symptoms include hip pain, clicking, and reduced hip joint function.
Hip Trauma
Hip trauma encompasses a range of injuries, including hip fractures, dislocations, and contusions. These injuries can result from accidents, falls, sports-related incidents, or other high-impact events. Hip trauma often requires immediate medical attention and may involve surgical intervention.
Avascular Necrosis
Avascular necrosis, also known as osteonecrosis, occurs when the blood supply to the hip joint is disrupted, leading to the death of bone tissue. This can result in hip pain and joint deterioration. Various factors, including injury, medication use, and certain medical conditions, can contribute to avascular necrosis.
Deep Gluteal Syndrome
Deep gluteal syndrome is a relatively uncommon condition characterised by pain in the deep buttock region. It can result from the compression of nerves, blood vessels, or other structures in the buttock area. This condition often requires a thorough evaluation to identify the underlying cause and appropriate treatment.
Trochanteric Bursitis
Trochanteric bursitis involves inflammation of the bursa sacs that cushion the greater trochanter, the bony prominence on the side of the hip. It can cause pain and tenderness on the outer hip and may be aggravated by walking or climbing stairs.
Diagnosis of Hip Conditions
- Medical History and Physical Examination: The diagnostic process often begins with a comprehensive medical history and a physical examination. Your healthcare provider will inquire about your symptoms, the duration of pain or discomfort, and any relevant medical conditions or injuries. During the physical examination, they will assess your hip's range of motion, strength, and stability.
- Imaging Studies: Imaging tests are crucial for assessing the structure and condition of the hip joint. Common imaging modalities include:
- X-rays provide detailed images of the bones and can help detect fractures, signs of arthritis, or structural abnormalities.
- MRI (Magnetic Resonance Imaging) scans offer a more in-depth view of soft tissues, including the cartilage, ligaments, and muscles. They are useful for diagnosing labral tears and other soft tissue injuries.
- CT (Computed Tomography) Scan may assess bone abnormalities and complex fractures.
- Blood Tests: In some cases, blood tests may be ordered to rule out systemic conditions such as autoimmune diseases or infections contributing to hip problems.
- Diagnostic Injections: In cases where the exact source of pain is unclear, diagnostic injections, such as hip joint or bursa injections, may be performed. These injections involve injecting medication directly into the affected area to pinpoint the source of pain and provide temporary relief.
- Arthroscopy: Arthroscopy is a minimally invasive surgical procedure that allows direct visualisation of the hip joint's interior. It is often used to diagnose and treat conditions like labral tears and femoroacetabular impingement.
Treatments for Hip Conditions
Treatment for hip conditions varies depending on the specific diagnosis and the severity of the condition. Here are some common treatment options:
- Conservative Measures:
- Physical therapy can help improve hip joint strength, flexibility, and mobility. Therapists design personalised exercise programs to address specific hip conditions.
- Non-steroidal anti-inflammatory drugs (NSAIDs) and pain relievers can help manage hip pain and inflammation.
- Adjusting daily activities, such as using assistive devices or avoiding activities that exacerbate symptoms, can be beneficial.
- Injections:
- Corticosteroid Injections can temporarily relieve inflammation and pain associated with conditions like bursitis or arthritis.
- In cases of osteoarthritis, hyaluronic acid injections may be used to improve joint lubrication and reduce pain.
- Surgical Interventions:
- Arthroscopic surgery diagnoses and treats certain hip conditions, including labral tears and femoroacetabular impingement.
- For severe hip arthritis or irreparable hip damage, total hip replacement surgery may be recommended. This involves replacing the damaged hip joint with an artificial one.
- Depending on the condition, surgical procedures like labral repair, osteotomy (bone realignment), or fracture repair may be necessary.