Knee Arthritis
What is Knee Arthritis?
Knee arthritis, also known as osteoarthritis of the knee or degenerative joint disease of the knee, is a degenerative joint disease that occurs when the protective cartilage in the knee joint breaks down, causing the bones to rub against each other. This leads to pain, stiffness, and inflammation in the knee joint.
Many conditions can cause arthritis, and the exact cause is often never known.
How Does Knee Arthritis Impact Your Anatomy and Health?
The knee joint is made up of three bones: the femur (thigh bone), the tibia (shin bone), and the patella (kneecap). The ends of these bones are covered with a smooth, protective layer of cartilage.
When knee arthritis occurs, the cartilage in the knee joint begins to wear away. This causes the bones to rub against each other, resulting in pain, swelling, and stiffness. Over time, the bone may deteriorate and develop bone spurs, making it difficult to move the knee joint.
Risk Factors for Knee Arthritis
While knee arthritis can affect anyone, certain risk factors increase the likelihood of developing the condition. These include
- Age: Knee arthritis is more common in older adults, particularly those over 50.
- Obesity: Excess weight stresses the knee joint, increasing the risk of knee arthritis.
- Gender: Women are more likely to develop knee arthritis than men.
- Genetics: There may be a genetic component to knee arthritis, as it tends to run in families.
- Previous knee injuries: Those who have suffered a knee injury, such as a fracture or ligament tear, are at higher risk for developing knee arthritis.
Causes of Knee Arthritis
The exact cause of knee arthritis is not fully understood, but several factors may contribute to its development. These include:
● Wear and tear: Over time, the protective cartilage in the knee joint may break down due to normal wear and tear.
● Inflammation: Chronic inflammation in the knee joint can lead to cartilage damage and eventually knee arthritis.
● Autoimmune disorders: In some cases, knee arthritis may be caused by an autoimmune disorder, such as rheumatoid arthritis.
● Injuries: A previous knee injury, such as a fracture or ligament tear, can increase the risk of developing knee arthritis later in life.
Symptoms of Knee Arthritis
The symptoms of knee arthritis may vary depending on the severity of the condition. Common symptoms of knee arthritis include
- Pain and tenderness in the knee joint
- Stiffness in the knee joint, particularly in the morning or after sitting for an extended period
- Swelling or inflammation in the knee joint
- A popping or cracking sound when bending the knee joint
- Limited range of motion in the knee joint
- A feeling of weakness or instability in the knee joint
Types of Knee Arthritis
There are three main types of knee arthritis:
- Osteoarthritis: This is the most common type of knee arthritis. It occurs when the protective cartilage in the knee joint breaks down due to wear and tear over time.
- Rheumatoid arthritis: This autoimmune disorder causes the body's immune system to attack the synovial membrane that lines the knee joint.
- Post-traumatic arthritis: This type of knee arthritis occurs after a traumatic injury to the knee, such as a fracture or ligament tear.
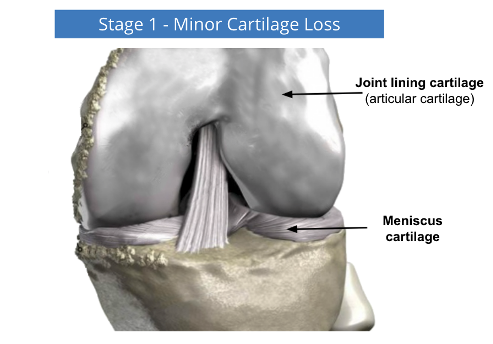
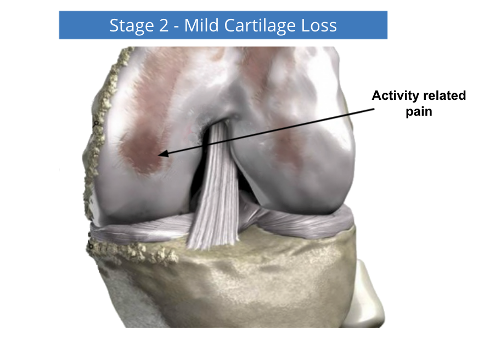
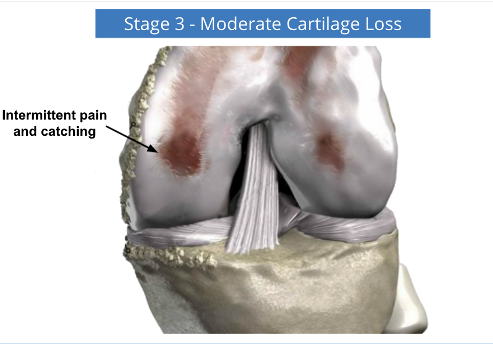
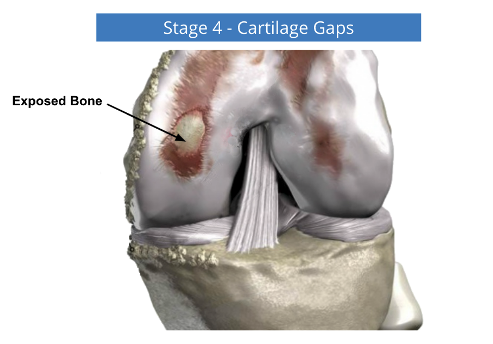
Stages of Knee Arthritis
The cartilage is a padding that absorbs stress.
The proportion of cartilage damage and synovial inflammation varies with the type and stage of arthritis. Usually, the pain early on is due to inflammation.
In the later stages, when the cartilage is worn away, most of the pain comes from the mechanical friction of raw bones rubbing on each other.
Diagnosis of Knee Arthritis
An orthopaedic surgeon can diagnose knee arthritis by physical examination and reviewing the patient's medical history. They may also recommend imaging tests, such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans, to evaluate the extent of cartilage damage in the knee joint.
What Can You Do?
Consult your doctor, who will determine the type of arthritis you have.
- Rest the joint until the pain subsides to prevent further inflammation
- To ease the pain or stiffness of the joint, apply heat on the joint for about 15 minutes once or twice a day using a hot water bottle, towel or an infrared lamp
- Take painkillers or anti-inflammatories, as recommended by your doctor
- If you are overweight, try to reduce weight to lighten the load on weight-bearing joints
- Participate in regular exercise
What Your Doctor Can Do For You?
The Doctor will need to take a personalised history and determine what is causing your pain and dysfunction and then determine an appropriate and responsible treatment plan. Treatment is a combination of education, physical and chemical interventions.
Non surgical treatment for Knee Arthritis
Initial treatment for knee osteoarthritis is conservative, consisting of rest, avoiding vigorous weight-bearing activities, and using non-narcotic analgesic and anti-inflammatory medications. With worsening symptoms, a cane or a knee brace may be helpful.
An injection of cortisone into the joint is frequently advised for more severe symptoms and can be beneficial.
Treatment of osteoarthritis focuses on decreasing pain and improving joint movement. It may include:
- Exercises to keep joints flexible and improve muscle strength
- Many different medications are used to control pain, including corticosteroids and NSAIDs and Paracetamol
- Glucocorticoids injected into joints that are inflamed and not responsive to NSAIDS
- Hyaluronic Acid injections
- Heat/cold/compression/electrical therapy for temporary pain relief
- Offloading braces or custom braces
- Weight control to prevent extra stress on weight-bearing joints
Surgery for Knee Arthritis
When conservative measures have been exhausted, offer no relief and have become disabling, surgery may be recommended. Different surgical procedures can be used and may include:
Synovectomy
This surgery is usually indicated for early cases of inflammatory arthritis where there is significant swelling (synovitis) that is causing pain or limiting the range of motion.Synovectomy is the surgical removal of the inflamed synovium (the tissue lining the joint). It may be performed using arthroscopy.
Arthroscopy
Keyhole surgery to debride cartilage flaps, remove loose bodies and trim meniscal tears can reduce the irritation and inflammation of arthritis.
Knee Osteotomy - knee preservation surgery
Knee osteotomy has three goals:
- To transfer weight from the arthritic part of the knee to a healthier area
- To correct poor knee alignment
- To prolong the life span of the knee joint
Advantages of the procedure include the following:
- By preserving your own knee anatomy, a successful osteotomy may delay the need for a joint replacement for several years.
- There are no restrictions on physical activities after an osteotomy has healed — you will be able to participate in your favourite activities, even high-impact exercise.
Osteotomy does, however, have some disadvantages:
- Pain relief is not as predictable after osteotomy compared with a partial or total knee replacement.
- Recovery from osteotomy is typically longer and more difficult because you may not be able to bear weight on your operated knee right away. The osteotomy needs time to heal, which takes approximately 6 weeks.
Procedure
In a tibial osteotomy, a wedge of bone is removed to straighten out the leg.
Most osteotomies for knee arthritis are done on the tibia (shinbone) to correct a bowlegged alignment that is putting too much stress on the inner (medial) compartment of the knee.
Tibial osteotomy was first performed in Europe in the late 1950s and brought to the United States in the 1960s. This procedure is sometimes called a high tibial osteotomy (HTO).
Arthroplasty - Joint resurfacing
In this procedure, your surgeon removes the affected joint and replaces it with an artificial implant. It is usually performed when the joint is severely damaged by osteoarthritis, rheumatoid arthritis, post-traumatic arthritis or avascular necrosis.
The goal of the surgery is to relieve pain and restore the normal functioning of the joint. Total joint or Partial Joint replacement can be performed through an open or minimally invasive approach.
Your surgeon will discuss these options with you and help you decide which type of surgery is most appropriate for you.
Does Exercise Help Those Who Have Knee Arthritis?
Exercise is essential because it increases the lubrication of the joints and strengthens the surrounding muscles, putting less stress on joints.
Exercise in heated swimming pools (hydrotherapy) can greatly relieve pain and stiffness.
Studies have also shown that exercise helps people with arthritis by reducing joint pain and stiffness and increasing flexibility, muscle strength, and energy. It also helps with weight reduction and offers an improved sense of well-being.