Partial Knee Replacement
What is a Partial Knee Replacement?
Partial Knee Replacement is also known as Single Compartment Knee Replacement, Unicompartmental Knee Replacement, or Unicondylar Knee Replacement.
Your knee can be divided into three compartments:
- Patellofemoral, the compartment in front of the knee between the knee cap and thigh bone,
- Medial compartment, on the inside portion of the knee, and
- Lateral compartment, which is the area on the outside part of the knee joint.
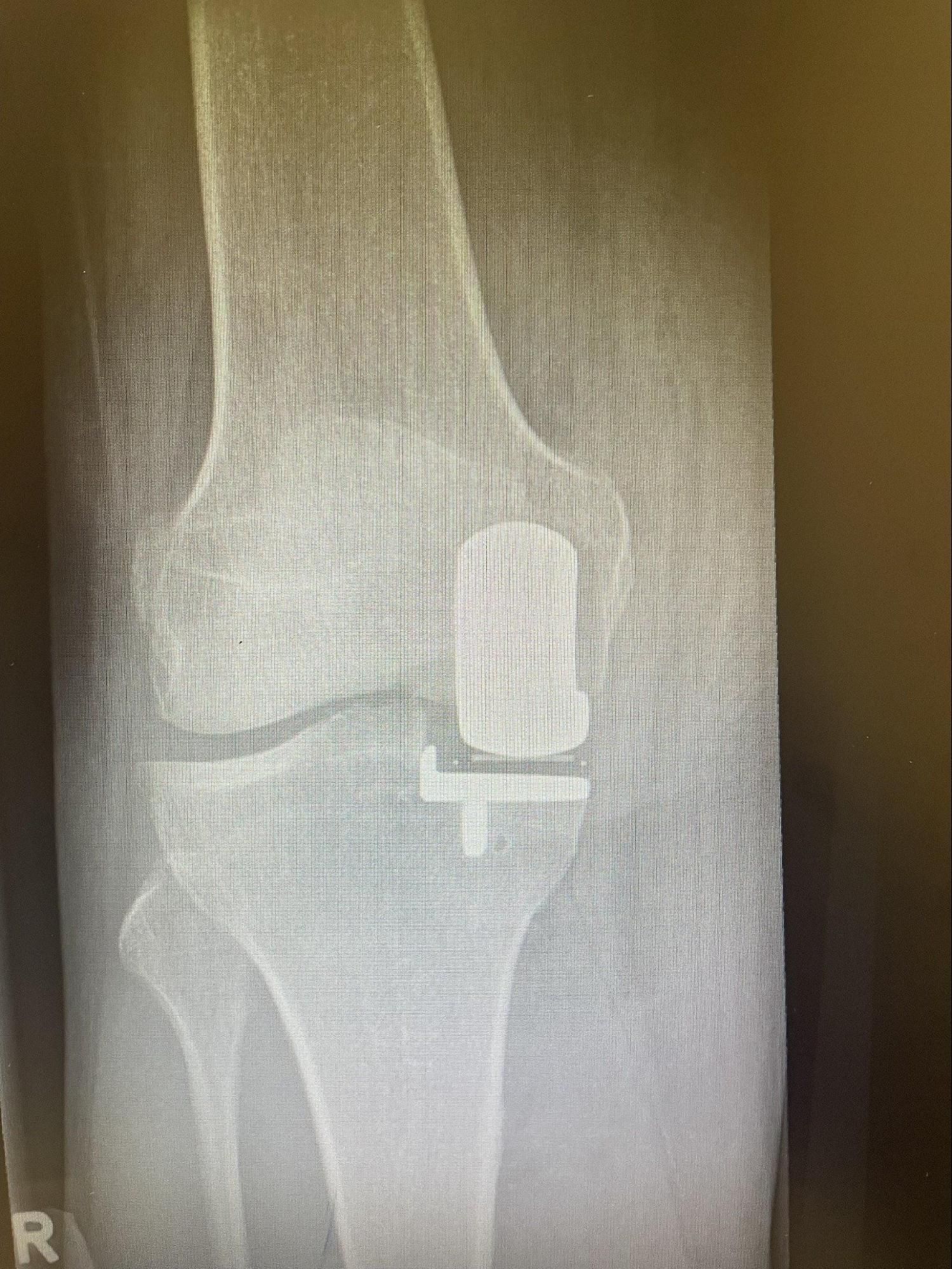
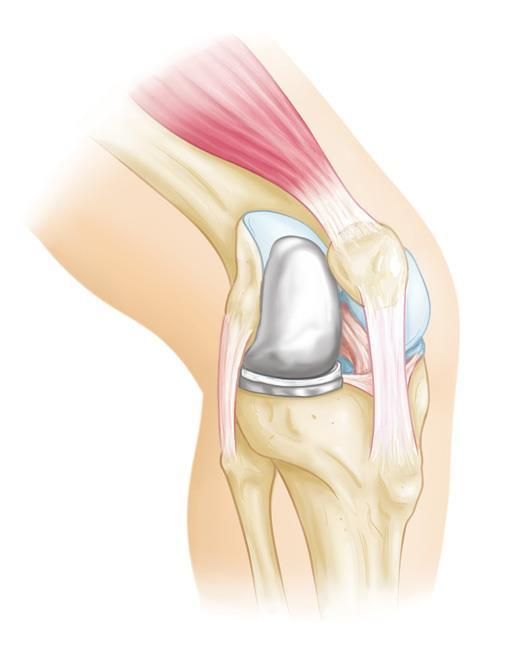
Sometimes, the damage to your knee is limited to only one compartment. A Partial Knee Replacement surgery is performed to replace only the worn-out parts of your knee with metal and plastic implants. If more than one compartment of your knee is worn out, a total knee replacement surgery may be needed instead.
Who Is Suitable for Partial Knee Replacement?
Patients ideal for partial (unicompartmental) knee replacement are those with damage localised to one area of the joint, normal ligaments in the knee, and minimal deformity or previous trauma to the knee. In cases where arthritis within the knee is too widespread, a total knee replacement is considered.
Knee Surgery Recommendation
Once you and your doctor have agreed on knee replacement surgery, your doctor will often discuss the options available and the patient’s preferences. These may include the following:
- Specific surgery type. (Partial Knee Replacement- if suitable vs Total Knee Replacement)
- Knee implant (fixed vs mobile bearing)
- Surgical technique (Robotic-assisted, Navigated, PSI- Patient Specific Instrumentation or conventional instruments)
These recommendations and the ideal approach to the knee depend on the individual patient’s anatomy, and your doctor will advise you of the most appropriate partial knee replacement and surgical technique.
We aim to return patients to their previous activity level with a fully functioning, pain-free knee joint.
Benefits of Partial Knee Replacement
Partial knee replacement offers several benefits for eligible candidates:
- Preservation of Healthy Tissue: Unlike total knee replacement, which involves removing all knee joint surfaces, partial knee replacement preserves the healthy portions of the knee. This means less disruption to the natural anatomy, potentially resulting in a more natural-feeling knee.
- Faster Recovery: The recovery time for partial knee replacement is often shorter than total knee replacement. Patients typically experience less pain and can return to their daily activities sooner.
- Improved Range of Motion: Many patients report improved knee function and a better range of motion following partial knee replacement.
- Less Blood Loss: Partial knee replacement generally involves less blood loss during surgery than total knee replacement.
- Lower Risk of Complications: Due to its less invasive nature, partial knee replacement carries a lower risk of certain complications, such as infection and blood clots, than total knee replacement.
Types of Partial Knee Replacement
There are different types of partial knee replacement procedures, each targeting a specific compartment of the knee:
- Medial Compartment Knee Replacement: This is the most common type of partial knee replacement. It addresses arthritis or damage in the inner part of the knee joint.
- Lateral Compartment Knee Replacement: This procedure treats issues in the knee joint's outer part.
- Patellofemoral Compartment Knee Replacement: When the front of the knee joint is affected, patellofemoral compartment knee replacement may be recommended.
How is a Partial Knee Replacement Performed?
Technology has improved partial knee replacement with the utilisation of robotics. This advanced technology allows for high levels of accuracy in operative planning, bone resection measurement, and component sizing. A pre-operative CT scan is performed. This allows for three-dimensional measurements and a plan for component size and placement. The Mako robotic arm then helps achieve accurate component implantation, position, and ligament balancing.

What to Do Before a Partial Knee Replacement
- Consultation and Evaluation: During this consultation, your surgeon will assess your knee, review your medical history, and conduct necessary tests, such as X-rays or MRI scans, to determine the extent of your knee damage and whether you are a suitable candidate for the procedure.
- Medication Review: It is important to discuss your current medications with your doctor. Some medicines may need to be adjusted or temporarily discontinued before the surgery.
- Physical Therapy: Engaging in physical therapy exercises before the surgery can help strengthen the muscles around your knee joint and improve your range of motion, facilitating a smoother recovery process.
- Home Preparation: Consider adjustments at home to ensure a safe and comfortable recovery. This may include installing handrails, securing rugs, and rearranging furniture to minimise tripping hazards.
- Assistance and Support: Arrange for a friend or family member to assist you during the initial days following the surgery. You may need help with daily tasks like cooking, cleaning, and transportation.
Partial Knee Replacement Procedure
Partial (unicompartmental) knee replacement is designed to allow a faster return to activity and maintain a ‘natural’ feeling knee.
- First, a small incision is made to expose the knee joint. The damaged bone and cartilage on the medial or lateral side (or patellofemoral) are removed with specialised cutting jigs and guides.
- Trial components are inserted to check the accuracy of cuts and ensure optimal joint alignment.
- The definitive components are then inserted with or without cement, and the damaged knee is replaced with metal components (tibia and femur) and a plastic bearing between.
Post-Op Care After Partial Knee Replacement
Pain Management
Your pain will vary depending on the individual; however, most patients find that pain is manageable from the smaller incision and less damaged bone requiring replacing. Usually, patients will initially require regular pain relief consisting of paracetamol and anti-inflammatories if indicated. Faster-acting pain medication will be given for periods of increased pain during the day (breakthrough pain). Like any medication, there can be side effects such as nausea, stomach upset or sedation. However, doses can be reviewed to ensure comfort and reduce these side effects. Ice and knee elevation every two hours are also recommended to help with swelling and pain.
Mobility
While in the hospital, a physiotherapist will visit you regularly to give you exercises and assist you in your return to walking. Full weight-bearing and walking are allowed immediately, initially with crutches. Most people can walk independently 10-14 days post-operation. You must perform the prescribed exercises to ensure optimal recovery.
Management of swelling by regularly applying ice and elevating the knee is also important to reduce swelling and regain movement in the knee.
Return to Work and Sport
Your return to work will vary depending on the procedure and work type. A minimum of 4 weeks off work should be taken to allow your incision to heal and mobility to improve. You may require up to 6 weeks for labour-intensive work before returning to full duties.
During this period, patients are not fit to perform duties that include:
- Prolonged standing
- Heavy lifting
- Bending or,
- Excessive stair climbing
Low-impact activities such as cycling and swimming/hydrotherapy can be commenced from week 4 and are also recommended to help increase muscle strength and function. High-impact activities such as running and jumping are best avoided for 8-12 weeks post-operation.
Partial Knee Replacement Prognosis
The prognosis following a partial knee replacement is generally positive for eligible candidates who undergo the surgery. Here are some key points to consider:
- Pain Relief: One of the primary goals of partial knee replacement is to alleviate pain and improve knee function. Many patients experience a substantial reduction in pain and an improvement in their ability to perform daily activities.
- Improved Mobility: Partial knee replacement can lead to increased joint mobility and a better range of motion in the affected knee. This can enhance overall quality of life and the ability to engage in physical activities.
- Longevity of Implants: The artificial implants used in partial knee replacement are designed to be durable and long-lasting. However, the longevity of the implants can vary from person to person, and factors such as age, activity level, and implant type can influence their lifespan. 70% of partial knee replacements last 25 years.
- Success Rate: Partial knee replacement is highly successful when performed on appropriate candidates. Success is typically defined as improved pain relief and functionality.
- Patient Satisfaction: Many individuals who undergo partial knee replacement report high satisfaction with the procedure, as it can significantly improve their quality of life.
Partial Knee Replacement Risks
Like any surgical procedure, partial knee replacement carries risks, though they are less than total knee replacement. It is important to be aware of these risks when considering the surgery:
- Infection: Infection is a possible complication of any surgery. The risk is minimised through strict adherence to sterile techniques during the procedure and antibiotics before and after surgery.
- Blood Clots: The immobility associated with the recovery process can increase the risk of blood clots forming in the legs (deep vein thrombosis) or travelling to the lungs (pulmonary embolism). Blood-thinning medications and early mobilisation are used to mitigate this risk.
- Implant Issues: While implant failure or loosening is rare, it can occur over time. This may necessitate revision surgery to replace or adjust the implant.
- Pain and Stiffness: Some patients may experience persistent pain or stiffness after surgery. This can often be managed with physical therapy and pain medications.
- Nerve or Blood Vessel Injury: Although rare, injury to nearby nerves or blood vessels can occur during surgery. Surgeons take precautions to minimise this risk.
- Allergic Reaction: Some individuals may have allergic reactions to the materials used in the implants. This is uncommon but should be discussed with your surgeon.
- Failure to Alleviate Pain:
In some cases, partial knee replacement may not provide the expected pain relief or functional improvement. It is important to have realistic expectations and discuss potential outcomes with your surgeon.