Trochanteric Bursitis
What is Trochanteric Bursitis?
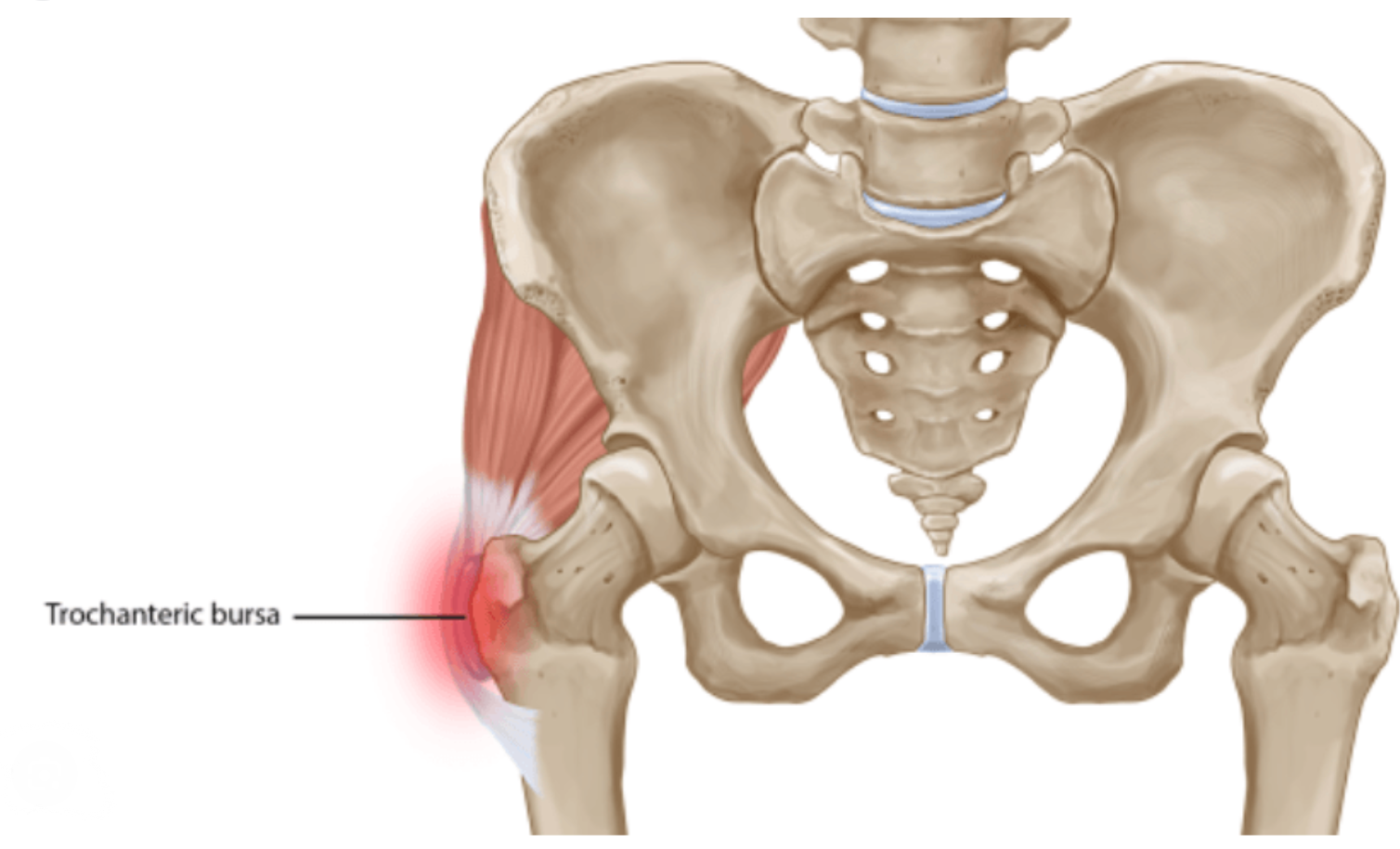
Trochanteric bursitis is a condition characterised by inflammation of the bursa located near the greater trochanter of the femur, the bony prominence on the outside of the hip. The bursa is a small, fluid-filled sac that acts as a cushion between the bone and the surrounding soft tissues, such as muscles, tendons, and skin. Its role is to reduce friction and provide smooth movement between these structures.
How Does Trochanteric Bursitis Impact Your Anatomy and Health?
Trochanteric bursitis typically presents with pain on the outside of the hip. This pain may radiate down the thigh or buttock and can worsen with walking, climbing stairs, or lying on the affected side. It may be sharp or dull and worsen at night, especially when lying on the affected side.
The inflammation of the trochanteric bursa can limit hip mobility and make it difficult to perform daily activities involving hip movement. Patients may experience stiffness and reduced range of motion in the hip joint, which can affect their ability to walk, stand, or engage in physical activities.
Causes and Risk Factors for Trochanteric Bursitis
Several factors can increase the risk of developing trochanteric bursitis:
- Repetitive Activities: Engaging in repetitive activities that stress the hip joint, such as running, cycling, or stair climbing, can increase the risk of irritation and inflammation of the trochanteric bursa.
- Hip Injuries: Trauma or injury to the hip, such as a fall or direct blow to the hip region, can damage the trochanteric bursa and lead to inflammation.
- Muscle Imbalances: Weakness or tightness in the muscles around the hip joint, including the gluteal muscles and hip abductors, can alter biomechanics and increase pressure on the trochanteric bursa, predisposing it to inflammation.
- Obesity: Excess body weight can place increased stress on the hip joint and bursa, contributing to the development of trochanteric bursitis.
- Age: Older adults are more prone to developing trochanteric bursitis due to age-related changes in joint structures and increased likelihood of degenerative conditions such as osteoarthritis.
- Previous Hip Surgery: Individuals who have undergone hip surgery or procedures involving the hip joint may have an increased risk of developing trochanteric bursitis due to alterations in joint mechanics and tissue healing.
- Certain Medical Conditions: Conditions such as rheumatoid arthritis, gout, or spinal conditions affecting the lower back and pelvis can increase the risk of developing trochanteric bursitis.
- Poor Posture: Incorrect posture or biomechanical abnormalities can strain the hip joint and bursa excessively, leading to inflammation over time.
- Leg Length Discrepancy: A difference in leg length can alter gait mechanics and increase pressure on one hip, potentially leading to trochanteric bursitis on the affected side.
Symptoms of Trochanteric Bursitis
- Hip Pain: Pain is the primary symptom of trochanteric bursitis and is typically localised to the outer side of the hip. The pain may also radiate down the thigh or buttock and can vary in intensity from mild to severe.
- Tenderness: The affected area may be tender to touch, especially over the greater trochanteric bursa. Pressing on the outer side of the hip may elicit pain or discomfort.
- Pain with Movement: Activities that involve movement of the hip joint, such as walking, climbing stairs, or standing up from a seated position, can exacerbate pain in individuals with trochanteric bursitis.
- Stiffness: Patients may experience stiffness or limited range of motion in the hip joint, particularly upon waking in the morning or after prolonged periods of inactivity.
- Worsening Pain at Night: Pain from trochanteric bursitis may worsen at night, especially when lying on the affected side. This can interfere with sleep and affect overall comfort.
- Difficulty Sitting or Lying on the Affected Side: Individuals with trochanteric bursitis may find sitting or lying on the affected side uncomfortable due to increased pressure on the inflamed bursa.
- Swelling: In some cases, there may be mild swelling or inflammation around the outer hip region, although this is less common compared to other symptoms.
- Pain with Palpation: doctors may elicit pain or discomfort upon palpation of the greater trochanteric bursa during physical examination.
Diagnosis of Trochanteric Bursitis
The following diagnostic methods may be used for the diagnosis of trochanteric bursitis:
- Medical History: Your doctor will ask about your symptoms, medical history, and any factors contributing to hip pain, such as recent injuries, repetitive activities, or underlying medical conditions.
- Physical Examination: During the physical examination, your doctor will assess the range of motion of your hip joint, palpate the outer hip region for tenderness or swelling, and perform specific manoeuvres to reproduce pain associated with trochanteric bursitis.
- Imaging Studies: While not always necessary, imaging studies such as X-rays, ultrasound, or magnetic resonance imaging (MRI) may be ordered to rule out other potential causes of hip pain, such as fractures, arthritis, or tendon injuries. These imaging modalities can also help visualise the size and condition of the trochanteric bursa and surrounding structures.
- Diagnostic Injections: In some cases, your doctor may recommend a diagnostic injection of a local anaesthetic, such as lidocaine, into the trochanteric bursa. If the injection temporarily relieves symptoms, it can help confirm the diagnosis of trochanteric bursitis.
- Laboratory Tests: Blood tests may be ordered to rule out underlying inflammatory conditions or infections contributing to hip pain, although these are typically not specific for diagnosing trochanteric bursitis.
Treatment Options for Trochanteric Bursitis
- Rest and Activity Modification: Resting the affected hip and avoiding activities that exacerbate symptoms, such as running or climbing stairs, can help reduce inflammation and promote healing. Modify activities to minimise stress on the hip joint and gradually reintroduce them as symptoms improve.
- Ice Therapy: Applying ice packs to the outer hip region for 15-20 minutes several times a day can help reduce pain and inflammation. Wrap the ice pack in a cloth to protect the skin and avoid prolonged exposure to prevent frostbite.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs, such as ibuprofen or naproxen, can help relieve pain and reduce inflammation associated with trochanteric bursitis. Follow the recommended dosage and consult with a healthcare professional, especially if you have any underlying medical conditions.
- Physical Therapy: A structured physical therapy program can help strengthen the muscles around the hip joint, improve flexibility, and correct biomechanical issues that may contribute to trochanteric bursitis. The treatment plan may include therapeutic exercises, stretching, manual therapy, and modalities such as ultrasound or electrical stimulation.
- Corticosteroid Injections: In cases of persistent or severe pain, corticosteroid injections may be administered directly into the trochanteric bursa to reduce inflammation and temporarily relieve symptoms. For accuracy, these injections are typically performed under ultrasound or fluoroscopic guidance.
- Ultrasound-Guided Needle Aspiration: In some cases, fluid may accumulate within the inflamed trochanteric bursa, causing pain and discomfort. Ultrasound-guided needle aspiration can drain excess fluid from the bursa, relieving pressure and alleviating symptoms.
- Biomechanical Assessment and Orthotics: Addressing underlying biomechanical issues, such as muscle imbalances or gait abnormalities, through customised orthotics or footwear modifications can help improve hip alignment and reduce stress on the trochanteric bursa.
- Activity Modification and Ergonomics: Adjusting work or daily activities to minimise repetitive movements or prolonged standing can help prevent the worsening of symptoms and promote the healing of trochanteric bursitis.